Patient education
Ovulatory / hormonal bleeding
Not all abnormal bleeding is caused by something “growing” in the uterus. Often the issue is how hormones and ovulation are behaving (or not behaving). This page explains what that means, how we assess it, and links to deeper pages for the common underlying causes.
Quick take
If bleeding is unpredictable (irregular timing), prolonged, or happens after long gaps without a period, ovulation may be inconsistent. That can lead to uneven thickening and shedding of the uterine lining, causing spotting or heavier bleeding.
What it is
“Abnormal uterine bleeding” means bleeding that’s abnormal in timing, amount, or duration. In reproductive-age patients it can be due to structural causes (like polyps or fibroids) or non-structural causes such as ovulatory dysfunction, endocrine issues, medications, or bleeding disorders.
Ovulatory / hormonal bleeding usually refers to bleeding driven by inconsistent ovulation (anovulation or oligo-ovulation). Without regular progesterone exposure, the lining can build up under estrogen and shed irregularly.
Normal cycle, in 20 seconds (optional)
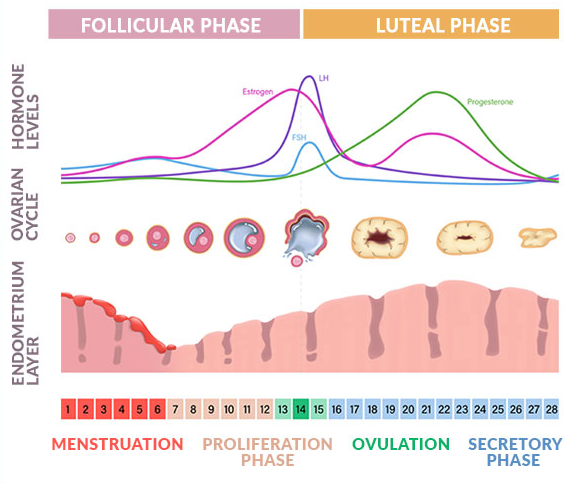
A typical cycle has two phases. In the first half, oestrogen helps the lining thicken. After ovulation, progesterone stabilises the lining. If pregnancy doesn’t happen, progesterone drops and the lining sheds as a period.
When ovulation is irregular or absent, progesterone is irregular too. The lining can build up and shed unevenly, which leads to unpredictable spotting, prolonged bleeding, or heavier bleeding after a long gap.
Patterns that suggest hormones
- Irregular timing (unpredictable cycles) is commonly linked to ovulatory dysfunction.
- Long gaps with no period, then spotting or heavy bleeding.
- Prolonged bleeding that drags on.
- Little or no cyclical “PMS-type” symptoms can happen when ovulation is inconsistent.
Common non-structural causes
Ovulatory dysfunction
- PCOS
- Thyroid disease or high prolactin
- Stress, weight loss, overtraining
- Perimenopause (cycle variability)
Medication & lining factors
- Hormonal contraception (unscheduled bleeding can occur)
- Anticoagulants
- Endometrial dysfunction / inflammation
More than one cause can exist at the same time. If bleeding persists despite treatment, we reassess for additional contributors.
How it’s diagnosed
- Pregnancy test in all reproductive-age patients with abnormal bleeding.
- Full blood count if bleeding is heavy/prolonged.
- TSH if thyroid disease is suspected.
- Prolactin if anovulation/amenorrhea or clinical suspicion.
- Androgens if signs of androgen excess (often in PCOS workup).
- Ultrasound when structural causes are possible or the pattern warrants imaging.
When we sample the lining
Hormonal bleeding is common and usually not cancer. But persistent irregular bleeding, especially with risk factors such as obesity or chronic anovulation, can increase risk because of prolonged unopposed estrogen exposure.
If bleeding persists or doesn’t respond as expected, we reassess and may recommend endometrial sampling (biopsy) depending on age, risk profile, and the overall pattern.
Treatment options
Treatment depends on whether pregnancy is desired, how heavy bleeding is, and what’s driving the pattern. Options include cycle regulation, bleeding reduction strategies, and addressing the underlying cause (for example PCOS or thyroid/prolactin issues).
Deep dives
These are separate pages with more detail. You can grow this list over time.
Perimenopause bleeding patterns
Cycle variability, missed ovulation, and when to investigate.
Stress / weight loss / overtraining
Hypothalamic cycle disruption and why periods can disappear.
FAQ
Is irregular bleeding always hormonal?
No. Structural causes (polyps/fibroids/adenomyosis) and cervix/vaginal causes can also cause spotting or irregular bleeding.
Do I always need an ultrasound?
Not always, but ultrasound is commonly used when structural causes are possible or the pattern warrants imaging.
Why do you do a pregnancy test even if I’m bleeding?
Because bleeding can happen in pregnancy too. Pregnancy should be excluded in all reproductive-age patients with abnormal bleeding.