Procedure
Hysteroscopy (Diagnostic & Operative)
Hysteroscopy is a camera procedure to look inside the uterus (womb) through the cervix. It can be used to diagnose problems causing bleeding, pain or fertility issues, and in many cases we can treat the problem during the same procedure.
A precise, minimally invasive approach
Hysteroscopy is “see-and-treat”. For many uterine problems, this is more accurate than blind procedures because we can directly visualise the cavity and target treatment (or biopsies) exactly where it’s needed.
When appropriate, we aim for the least invasive option that still gives a reliable diagnosis and a durable result.
What is hysteroscopy?
A thin telescope (camera) is gently passed through the vagina and cervix into the uterus to inspect the lining (endometrium). The uterus is distended with fluid so we can see clearly. Hysteroscopy can be done for diagnosis only, or with instruments to treat a problem during the same procedure.
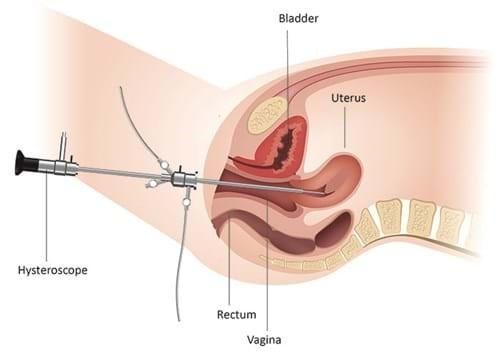
Key point: Hysteroscopy is performed through the cervix. There are no abdominal incisions.
Why is it done?
Hysteroscopy is most commonly used to evaluate symptoms or scan findings that suggest a problem inside the uterine cavity.
Abnormal bleeding
Heavy or irregular periods, bleeding between periods, or bleeding after menopause (where urgent evaluation is important).
Polyps or fibroids in the cavity
To confirm the diagnosis and remove lesions that contribute to bleeding, pain, or fertility problems.
Fertility / pregnancy-related indications
Selected cases of infertility, recurrent miscarriage, retained pregnancy tissue, or suspected cavity abnormalities.
Sometimes we recommend hysteroscopy after ultrasound or saline infusion sonography, especially when a targeted biopsy or treatment is likely.
Diagnostic vs operative hysteroscopy
Diagnostic hysteroscopy
- We inspect the cavity and identify abnormalities
- We can take targeted biopsies
- Often paired with endometrial sampling when needed
Operative hysteroscopy
- Polypectomy (removing polyps)
- Hysteroscopic myomectomy (selected fibroids)
- Adhesiolysis (scar tissue/Asherman’s)
- Removal of retained tissue or foreign bodies
“See-and-treat” advantage
When a lesion is visible, treating it under direct vision is typically more accurate than blind scraping (D&C). It also improves the quality of biopsies because sampling is targeted.
How it’s done (simple overview)
Step 1
Anaesthesia and positioning
Depending on the plan, hysteroscopy can be done under light sedation, spinal, or general anaesthesia. For operative procedures, general anaesthesia is common.
Step 2
Cervix preparation
The cervix is gently accessed. In some patients we use medication beforehand to soften the cervix, especially if the cervix is tight or prior access has been difficult.
Step 3
Camera inspection
We distend the cavity with fluid to see the lining clearly. The aim is a systematic inspection of the cavity and tubal openings.
Step 4
Treatment (if planned)
If an operative procedure is planned, specialised instruments are used to remove the lesion safely under direct vision. Tissue is sent to pathology when appropriate.
What matters most: choosing the right procedure for the right problem. Sometimes hysteroscopy is diagnostic only, and sometimes it’s the treatment.
How to prepare
Timing
For many patients, scheduling in the early part of the cycle can improve visibility. If you might be pregnant, we will confirm this before proceeding.
Medications
Tell us about blood thinners, diabetes medication, allergies and prior anaesthetic issues. Pain relief is usually simple and planned in advance.
What to expect
Light bleeding and cramping can occur afterwards. Most patients return to normal activities quickly, but operative procedures may need a short “take it easy” window.
Your exact preparation plan depends on whether this is diagnostic or operative, your cervix/uterine anatomy, and your medical history.
Risks & complications (plain language)
Hysteroscopy is generally safe, but risks depend on what is being done (diagnostic vs operative), the size/location of lesions, and individual anatomy.
- Bleeding (usually light, occasionally significant)
- Infection (uncommon)
- Cervical trauma or difficult access
- Uterine perforation (rare, more relevant in operative cases)
- Fluid-related complications (rare, monitored carefully)
- Need for further treatment if the lesion is large/complex
- Scar tissue formation (uncommon, situation-dependent)
- Anaesthetic risks (depend on health factors)
Safety focus: We monitor fluid balance during the procedure, use controlled energy when required, and choose the safest technique for the lesion and your anatomy.
Recovery & timelines
After diagnostic hysteroscopy
Often back to normal within 24 hours. Expect mild cramping and light spotting.
After operative hysteroscopy
Most patients recover quickly, but we may recommend a few days of lighter activity depending on what was done (polyp vs fibroid vs adhesions).
When to contact us
Heavy bleeding, fever, severe pain not improving, or feeling unwell after initial recovery should be assessed promptly.
FAQ
Is hysteroscopy the same as D&C?
No. A D&C is a “blind” scraping of the uterine lining. Hysteroscopy is visual inspection with a camera, and if we take tissue it can be targeted to the specific area of concern.
Will you always remove what you find?
If operative treatment is planned and safe, yes. But sometimes the safest plan is staged (for example large fibroids, difficult anatomy, or unexpected findings). We aim to avoid “heroic” surgery that creates problems later.
Will I get pathology results?
If tissue is removed or biopsied, it is typically sent for pathology. We’ll explain what was done and what the results mean.
Next steps
If hysteroscopy has been recommended, the next step is to confirm the goal: diagnosis, treatment, or both. In consultation we’ll review your symptoms, scans, and your priorities, then choose the safest plan that answers the question properly.
This page is general education. Your personalised plan depends on your diagnosis, anatomy, and overall health.