Treatment
Hysterectomy
A hysterectomy is surgery to remove the uterus (womb). For many conditions, it can be performed using minimally invasive techniques (vaginal or laparoscopic), which usually means less pain, fewer wound issues, and a faster recovery than open surgery.
A minimally invasive focus
When it’s appropriate and safe, I prioritise minimally invasive surgery. In general, vaginal hysterectomy is the preferred route when technically feasible, and if that’s not suitable, laparoscopic hysterectomy is usually the next option. Sometimes an open (abdominal) approach is still the safest choice, or may be needed unexpectedly.
This page is general education. Your plan depends on your diagnosis, anatomy, prior surgery, and your goals.
What is a hysterectomy?
A hysterectomy removes the uterus. Depending on the reason for surgery, it may also include removal of the cervix (total hysterectomy) or leaving the cervix in place (supracervical/subtotal hysterectomy). The ovaries and/or fallopian tubes are sometimes removed at the same operation if there’s a clear indication.
Important: After hysterectomy you can no longer carry a pregnancy. It does not automatically cause menopause unless the ovaries are removed.
Ovaries and fallopian tubes: what is removed, and why?
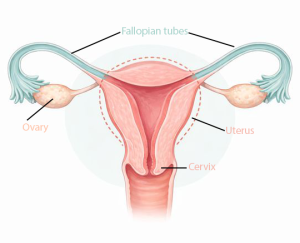
Illustration showing the uterus, cervix, fallopian tubes, and ovaries.
A hysterectomy removes the uterus. The fallopian tubes and ovaries are separate structures, and whether we remove them depends on your age, your diagnosis, your risk factors, and what we find at surgery.
Fallopian tubes (salpingectomy)
In many benign hysterectomies, we discuss removing the tubes while keeping the ovaries. The tubes are not needed after hysterectomy, and removal may reduce future risk of ovarian-type cancer.
Ovaries (oophorectomy)
Removing ovaries is considered when there is a clear reason (for example: cancer risk/pathway, abnormal ovaries, or specific endometriosis scenarios). If you are not menopausal, removing ovaries causes immediate menopause, so we weigh the pros and cons carefully.
How we decide
- Your age and menopausal status
- Your diagnosis (bleeding, endometriosis, prolapse, cancer pathway)
- Family history / genetic risk factors
- Ultrasound findings and what we see during surgery
In consultation we’ll decide together what should be removed and what should be preserved, and why. If ovaries are being removed, we’ll also discuss symptom management and hormone considerations where appropriate.
Who is a hysterectomy for?
A hysterectomy can be considered when symptoms are significant and other treatments are not suitable, haven’t worked, or aren’t desired. It’s used across multiple areas of gynaecology, including bleeding problems, endometriosis/adenomyosis, fibroids, prolapse surgery planning, and some cancer pathways (where appropriate staging and oncology input applies).
Because this page is linked from multiple conditions, I’ll keep the “why hysterectomy” decision focused and practical. In consultation, we’ll match the procedure to your diagnosis, your body, and your goals.
How we choose the surgical approach
There are three main routes: vaginal, laparoscopic (keyhole), and abdominal (open). Evidence-based guidance generally prioritises minimally invasive routes where feasible, with vaginal hysterectomy preferred when possible, and laparoscopic commonly the next alternative. Even with good planning, an abdominal incision may sometimes be needed to complete surgery safely.
Vaginal hysterectomy
Often the first choice when feasible. It is associated with strong outcomes and avoids abdominal incisions.
Laparoscopic (keyhole)
A minimally invasive option with small incisions. Compared with open surgery, it generally means shorter hospital stay and quicker return to normal activities.
Abdominal (open)
Sometimes the safest route, depending on anatomy, adhesions, uterine size, or surgical complexity. It can also be an unplanned “backup route” if needed during surgery.
How the route is decided: It’s based on what’s safest and most effective for your situation. Factors include uterine size and mobility, anatomy, prior pelvic surgery/adhesions, and whether additional procedures are planned.
How it’s done (simple overview)
Step 1
Anaesthesia + safety checks
General anaesthesia is most common. We confirm the plan, prevention of clots, and antibiotic cover as appropriate.
Step 2
Uterus is detached carefully
The uterus is separated from its attachments and blood supply in a controlled way, with care taken to protect the bladder, ureters, bowel, and pelvic nerves.
Step 3
Vaginal cuff closure
The top of the vagina is closed (“the cuff”). In selected cases, we also add support stitches to reduce future prolapse risk (see below).
Step 4
Recovery + discharge plan
Many minimally invasive hysterectomies can be done with short hospital stay, and in selected cases even same-day discharge.
Vault support (apex suspension): do I need it?
Removing the uterus can change how the top of the vagina is supported. In some situations, adding an apical support procedure at the time of hysterectomy can reduce the risk of future vault prolapse. The best “one-size-fits-all” approach is not known, so this is personalised.
If your support is normal
Routine prophylactic suspension is not always performed. If you have strong reasons to minimise future prolapse risk and accept the (small) added risks, it can be considered.
If you have prolapse symptoms or risk factors
Support procedures are discussed more actively when there are prolapse symptoms, asymptomatic prolapse, or risk factors like prior vaginal delivery, menopause, age, obesity, chronic constipation/cough, or previous pelvic surgery.
What it involves
Typically a native-tissue suspension (for example uterosacral ligament suspension or a McCall culdoplasty). This can improve apical support without introducing permanent mesh.
Bottom line: If prolapse is part of your story (or likely to become part of it), apical support is a key part of durable pelvic surgery planning, and we’ll decide together based on your exam and goals.
Risks & complications (plain language)
All surgery has risks. The exact risk depends on the route, your anatomy, previous surgery/adhesions, and what additional procedures are done.
- Bleeding (occasionally requiring transfusion or return to theatre)
- Infection
- Blood clots (DVT/PE) and the need for clot prevention
- Damage to nearby structures (bladder/ureter/bowel)
- For laparoscopic surgery: small risk of port-site complications
- Vaginal cuff issues (rare, but includes cuff dehiscence)
- Need to convert to open surgery in a minority of cases
- Ongoing pelvic symptoms depending on the original diagnosis
Notes: Laparoscopic hysterectomy can require conversion to open surgery (reported up to around a few percent in some series) and has recognised risks like urinary tract injury, cuff dehiscence, and bowel injury. Vaginal hysterectomy is generally preferred when feasible. Minimally invasive routes are prioritised when safe.
Recovery & timelines
Your recovery depends on the surgical route and what else is done at the same time (for example, prolapse repair or endometriosis excision). In general, minimally invasive approaches are associated with faster recovery than open surgery.
FAQ
- Will I go into menopause?
- Will my cervix be removed?
- Will sex feel different?
- Do I still need Pap smears?
- How long is recovery?
- Are there alternatives to hysterectomy?
FAQ
Will I go into menopause?
No, not automatically. Menopause is related to ovarian function. If your ovaries are kept, you do not enter immediate menopause because of hysterectomy. If the ovaries are removed and you are not already menopausal, you will enter immediate menopause.
FAQ
Will my cervix be removed?
Often yes (total hysterectomy), but not always. Keeping the cervix can be appropriate in selected cases. We’ll discuss what fits your diagnosis and anatomy.
FAQ
Will sex feel different?
Most women return to a normal sex life once healed. If heavy bleeding or pain were affecting intimacy, sex often improves. Healing time and the reason for surgery matter, so we’ll individualise guidance.
FAQ
Do I still need Pap smears?
It depends on whether your cervix is removed and your screening history. If the cervix remains, routine cervical screening continues. If the cervix is removed, screening may no longer be required in many cases, but exceptions exist (for example prior high-grade abnormalities). We’ll confirm your plan.
FAQ
How long is recovery?
Recovery depends on route and what else is done. Minimally invasive routes usually recover faster than open surgery. Your detailed guidance will be on the shared recovery page.
FAQ
Are there alternatives to hysterectomy?
Often yes. Alternatives depend on the diagnosis and may include medication, a Mirena IUD, hysteroscopy, endometrial ablation, fibroid treatments, or targeted endometriosis surgery. We’ll match options to your goals and risk profile.
Next steps
If hysterectomy is on the table, the goal is not “a bigger operation”, it’s the right operation. We’ll clarify the diagnosis, talk through alternatives, and then choose the safest route with the fastest recovery that still delivers a durable result.