Patient education
Abnormal uterine bleeding
If your bleeding interferes with your life, it deserves proper attention. This page helps you identify what might be causing it, how we investigate it, and what treatment options are available. Then you can click into the specific condition or treatment to learn more.
Browse the library
Short hub pages, detailed deep-dives. Useful when you’re reading now, and also useful later when we discuss options in consultation.
Tip: If you already know your diagnosis (eg fibroids), go straight to “Conditions”. If you want options (eg Mirena, ablation), go straight to “Treatments”.
Is this me?
Many women arrive here because something feels “off”. Common red flags include:
- Bleeding that soaks through pads/tampons very quickly
- Bleeding longer than 7–8 days
- Passing large clots regularly
- Needing double protection (pad + tampon)
- Bleeding between periods
- Bleeding after sex
- Cycles that are unpredictable or chaotic
- Fatigue, dizziness, or low iron symptoms
Practical test: if it disrupts work, exercise, travel, intimacy, sleep, or your confidence leaving the house, it deserves assessment.
When it’s urgent
Seek same-day care if you feel faint, short of breath, have chest pain, or you are soaking through pads hourly for several hours. Heavy bleeding can be medically significant.
How I assess abnormal bleeding
Step 1
Pattern + symptoms
We clarify what’s happening, how long it’s been going on, and whether anemia or pain is part of the picture.
Step 2
Examination
To confirm the source of bleeding and identify obvious cervical or vaginal causes.
Step 3
Ultrasound
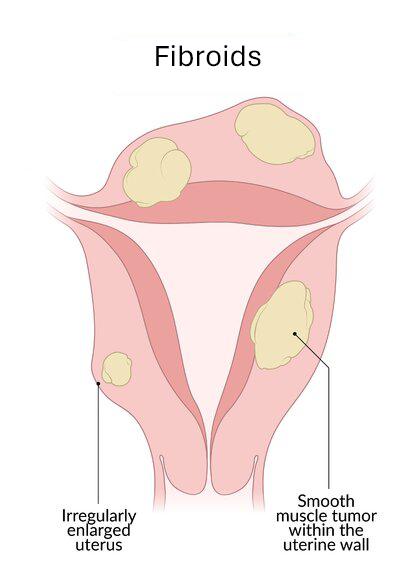
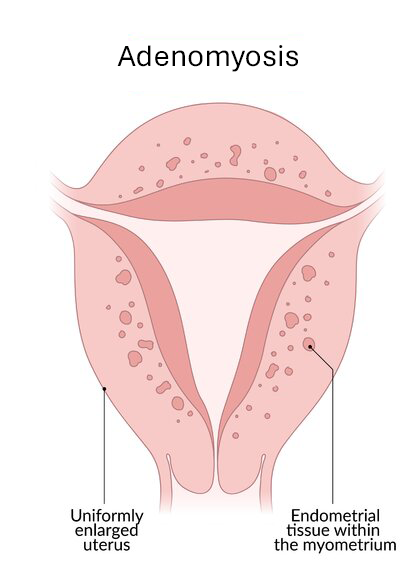
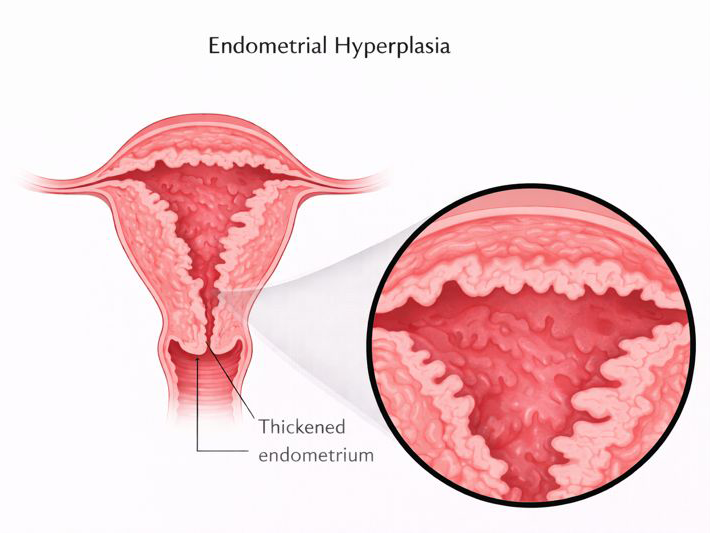
To assess the uterus and lining for fibroids, polyps, adenomyosis, and other structural issues.
Step 4
Targeted tests
Blood tests and endometrial sampling only when needed, based on your risk factors and bleeding pattern.
Common causes (conditions)
These pages explain what each condition is, how it’s diagnosed, and which treatment options typically apply.
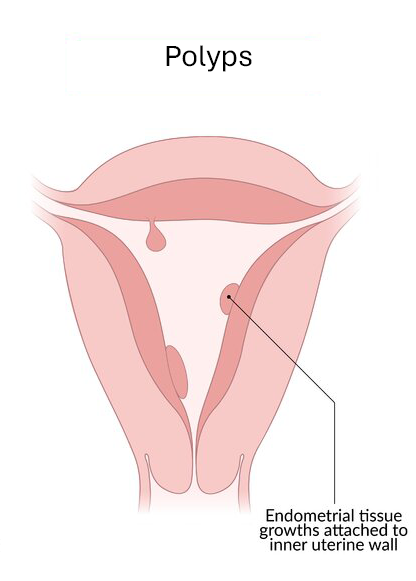
Endometrial polyps
Bleeding between periods, spotting, and targeted hysteroscopic treatment.
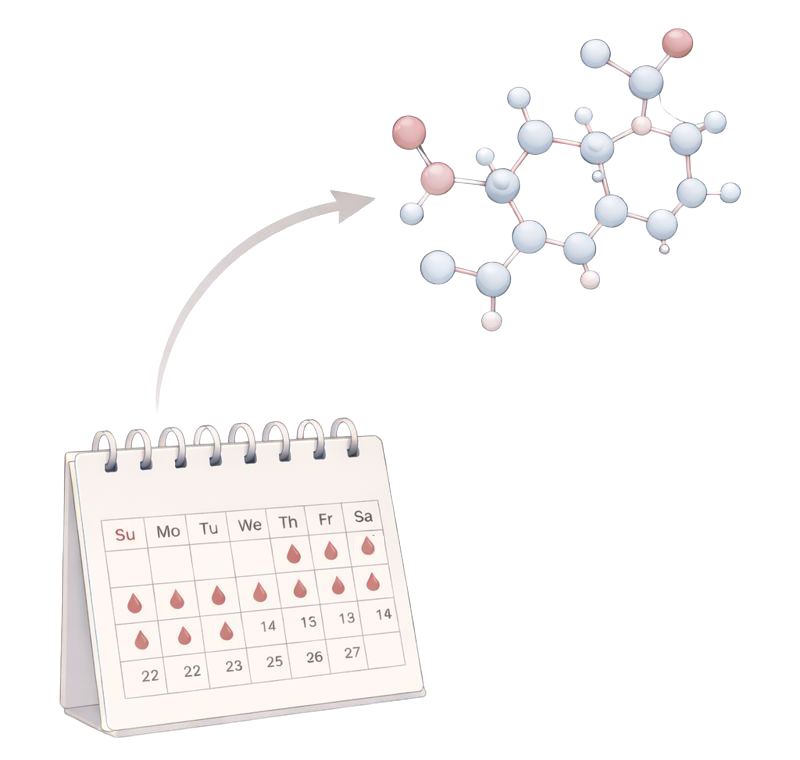
Ovulation / hormonal bleeding
Irregular cycles, perimenopause, PCOS, thyroid-related patterns.
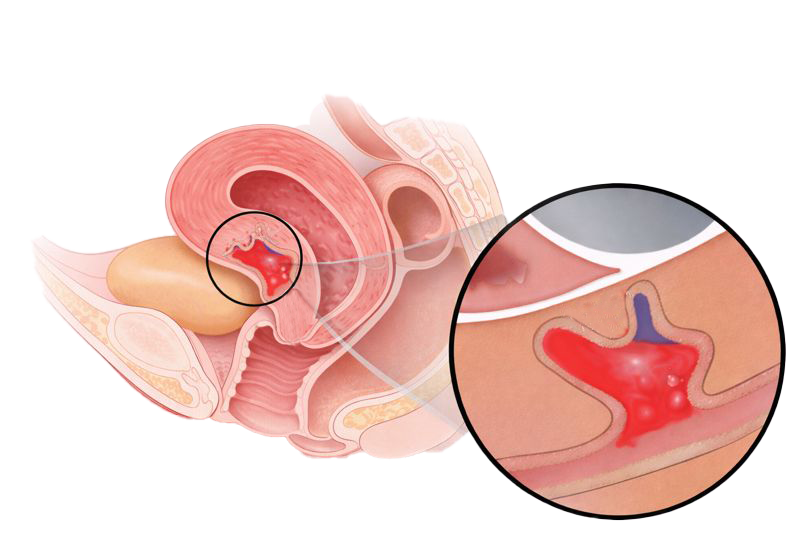
Cesarean scar defect (niche)
Post-menstrual spotting and “mysterious” persistent bleeding.
Treatment options
These pages explain each option clearly: who it’s for, what it involves, benefits, risks, and recovery. These can be linked from multiple conditions later.
Medical & hormonal options
Procedures & minimally invasive surgery
Minimally invasive surgery is a core focus of my practice. Where surgery is the right option, I prioritise techniques that reduce pain and recovery time while achieving a durable result.